Remplissage
Wolf et al [1] described the surgery in 2007 as an add-on to an arthroscopic anterior stabilisation procedure for the shoulder to address a significant engaging Hill-Sachs defect. When combined with arthroscopic Bankart repair, the Remplissage approach has been shown to reduce the frequency of recurrent anterior shoulder instability.
When the Hill-Sachs lesion is very big and 'engaged' the front glenoid with limited overhead movement, this approach is used (i.e.dislocating very easily due to the large Hill-Sachs lesion, as well as the Bankart lesion). In certain cases, a Bankart repair alone might not be enough. As a result, the method of remplissage evolved.
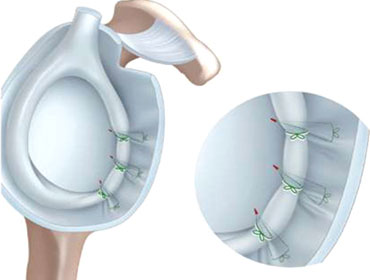
We've been doing the Remplissage operation since 2007, and we employ it once the Bankart lesion has been addressed. There are no more incisions (portals) made. The arthroscope is inserted through the anterior portal to examine the Hill-Sachs lesion on the humeral head's posterior surface. A burr is inserted through the posterior portal to decorticate the Hill-Sachs lesion. Through the posterior portal, a triple-loaded big rotator cuff anchor is placed into the Hill-Sachs defect. Sutures are threaded through the infraspinatus tendon and posterior capsule, then tied down with a 'parachute approach,' successfully filling the humeral head defect.